The human body is a highly sophisticated system where various processes work in harmony to maintain life and health. One such process that plays a vital role in the functioning of the reproductive system, particularly in women, is the egg deleup process. Though this term might seem unfamiliar, it refers to a series of events in female reproductive biology, specifically the development and maturation of eggs within the ovaries. This process is essential for fertility, hormonal balance, and overall reproductive health.
In this comprehensive analysis, we will explore the egg deleup process, its stages, how it affects the body, and its implications for fertility and overall health.
Understanding the Egg Deleup Process
Before diving into the specifics, it’s essential to define what the egg deleup process involves. The term “deleup” may not be commonly encountered in standard biological literature, but it is likely a variant or colloquial term referring to the development or maturation of eggs in the female reproductive system. The scientific term for this process is oogenesis—the development of ova (eggs) in the ovaries.

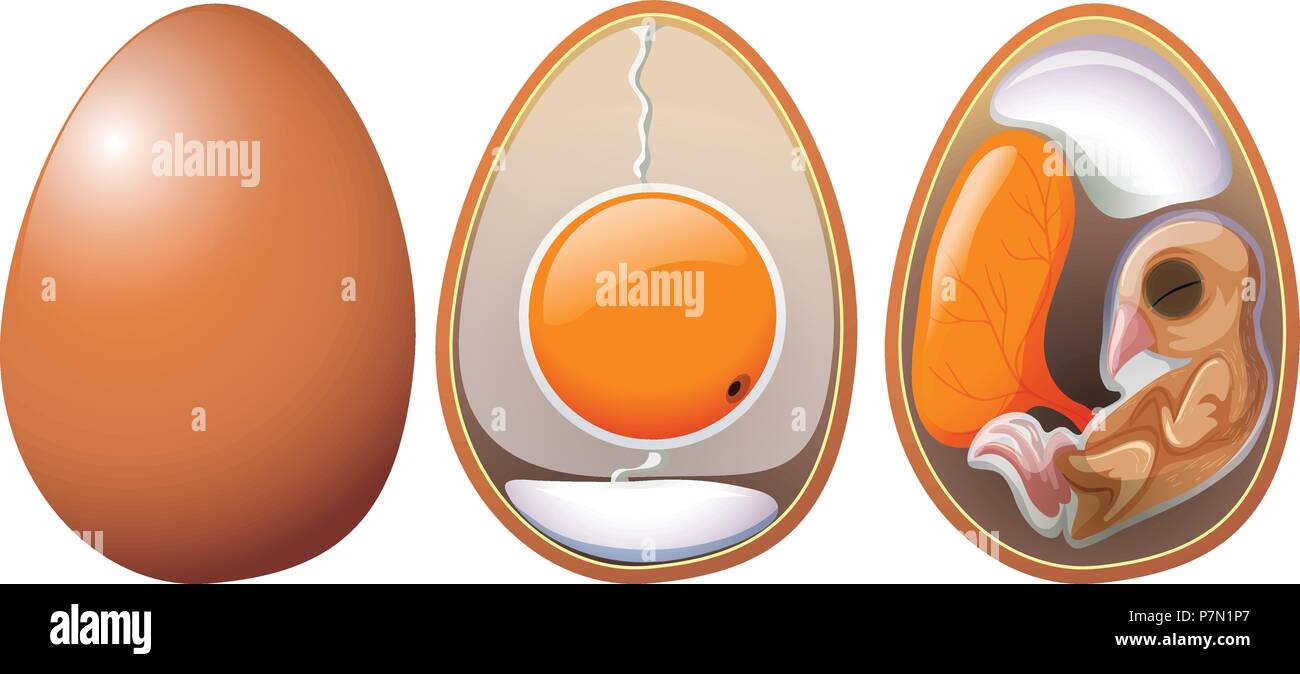
Oogenesis involves the creation, maturation, and release of eggs in response to hormonal signals from the brain. These eggs are the foundation of female fertility, and their maturation plays a central role in the ability to conceive. Every woman is born with a finite number of eggs, and over time, these eggs undergo a complex process of development, culminating in ovulation.
The Stages of the Egg Deleup (Oogenesis) Process
The egg deleup process is composed of multiple stages, which span from the formation of eggs during fetal development to the eventual release of a mature egg. Here is a breakdown of these stages:
1. Primordial Follicles: Early Stages of Egg Development
The process begins in the fetal stage when a female fetus develops a fixed number of primordial follicles—tiny sacs containing immature eggs or oocytes. These follicles are formed early in gestation, and the number of follicles a female has decreases as she ages, ultimately leading to menopause when follicular reserves are depleted. The primordial follicles remain dormant until puberty.
2. Puberty and Follicular Activation
At puberty, the hypothalamus in the brain starts releasing gonadotropin-releasing hormone (GnRH). This hormone stimulates the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones play a crucial role in the activation and recruitment of the primordial follicles for the next phase of development.
During the menstrual cycle, several follicles are recruited to begin maturing, though typically only one follicle will fully mature and release an egg (ovulation). As these follicles grow, they go through various stages, and the oocytes inside mature.
3. Primary Follicle to Secondary Follicle Stage
As the primordial follicles grow, they transition into primary follicles, characterized by a single layer of granulosa cells surrounding the oocyte. These follicles then develop into secondary follicles, where the granulosa cells multiply and the follicles begin producing estrogen, a key hormone involved in regulating the menstrual cycle.
The growth of the secondary follicle is marked by the development of a fluid-filled cavity called the antrum. The oocyte inside continues to mature, and as estrogen levels rise, they signal the body to prepare for ovulation.
4. Tertiary Follicle and Ovulation
The next stage is the development of the tertiary follicle, also known as a Graafian follicle. At this point, the follicle is ready to undergo ovulation. As it matures, the follicle swells and produces even more estrogen. This hormonal surge triggers a dramatic event in the cycle: the release of the egg.
The LH surge induced by estrogen causes the mature follicle to rupture and release the egg into the fallopian tube in a process known as ovulation. The egg is now ready to be fertilized if sperm is present. If fertilization does not occur, the egg disintegrates and is absorbed by the body.
5. Corpus Luteum Formation
After the egg is released, the remnants of the follicle transform into the corpus luteum, a structure that secretes progesterone, a hormone that helps prepare the uterus for potential implantation of a fertilized egg. If pregnancy does not occur, the corpus luteum will degenerate, leading to a drop in progesterone and the onset of menstruation. This process begins a new menstrual cycle, and the cycle of egg development starts again.
How the Egg Deleup Process Affects the Body
The egg deleup process has profound effects on a woman’s body, particularly in terms of hormonal regulation, fertility, and reproductive health.
1. Hormonal Regulation
The hormonal interplay during the egg development process is crucial for overall health. The hormones FSH, LH, estrogen, and progesterone fluctuate throughout the menstrual cycle and regulate not only the development and maturation of eggs but also other physiological processes, such as menstrual regularity and bone health.
Estrogen is particularly important as it helps maintain the health of the uterine lining, while progesterone prepares the body for pregnancy by thickening the uterine lining. A disruption in the balance of these hormones can lead to irregular periods, anovulation (lack of ovulation), or infertility.
2. Fertility and Reproductive Health
The primary role of the egg deleup process is, of course, fertility. Healthy egg development is essential for conception, as the release of a mature, viable egg is necessary for fertilization. As women age, the number and quality of their eggs decline, often leading to decreased fertility. Additionally, the egg’s ability to fertilize and develop into a viable embryo diminishes with age, which is why fertility tends to decrease in women after their mid-30s.
Health conditions such as polycystic ovary syndrome (PCOS), endometriosis, and ovarian insufficiency can disrupt the egg development process and lead to difficulties with conception. Regular monitoring of reproductive health through medical examinations can help detect any abnormalities early on, providing women with the opportunity to address fertility challenges of egg deleup process.

3. Menstrual Cycle and Ovulation
The egg deleup process is tightly linked to the menstrual cycle. A healthy cycle is typically around 28 days, although it can vary. The development of the egg follows a pattern in the first half of the cycle, while ovulation occurs around the middle. The second half of the cycle involves the luteal phase, where the corpus luteum produces progesterone in preparation for a possible pregnancy. If the egg is not fertilized, menstruation occurs, signaling the start of a new cycle.
This cyclical process is essential for the functioning of the female reproductive system. When disruptions occur—whether from stress, hormonal imbalances, or medical conditions—it can affect fertility and general health.
The Impact of Lifestyle Factors on the Egg Deleup Process
Many external factors can influence the egg deleup process, affecting the quality and number of eggs a woman has. These factors include:
- Age: As previously mentioned, egg quality and quantity naturally decline with age, especially after the age of 35. Women are born with all the eggs they will ever have, and by puberty, the number has already significantly reduced.
- Diet and Nutrition: Proper nutrition is essential for hormone regulation. A balanced diet rich in antioxidants, healthy fats, and vitamins can support ovarian health and egg quality.
- Exercise: Regular exercise helps maintain a healthy weight and balances hormone levels, both of which are important for fertility.
- Stress: Chronic stress can negatively impact hormonal levels and disrupt ovulation, making it harder to conceive.
- Environmental Factors: Exposure to environmental toxins, such as endocrine disruptors in plastics or chemicals, can interfere with hormone production and egg development.
Conclusion
The egg deleup process (oogenesis) is a complex yet fundamental part of the female reproductive system. It governs the maturation of eggs in the ovaries, facilitating the reproductive cycle and influencing fertility. Through the precise orchestration of hormonal signals, this process ensures that the body is capable of producing viable eggs that can lead to pregnancy. Understanding the various stages of egg development, as well as the factors that can impact this process, is key to maintaining reproductive health and managing fertility.
As we learn more about this intricate biological process, it becomes clear that the health of the eggs is essential not only for reproduction but also for overall well-being. By adopting a healthy lifestyle and being mindful of factors that affect the egg deleup process, women can take proactive steps toward supporting their reproductive health and ensuring optimal fertility.